Vitamin D beats the vaccines against COVID; Part 3 of a series
Whereas vaccines only work on adaptive, not innate immunity, vitamin D stimulates, coordinates and strengthens the entire immune system. Part 3 of a series.
© Colleen Huber, NMD
Adaptive immunity and the COVID vaccines
The adaptive immune system comprises T-cells and B-cells (lymphocytes), and it is the smaller part of the human immune system. I say this because T-cells and B-cells are less than 30% (with wide variation in individuals) of the white blood cells in a complete blood count, and are less than two tenths of one percent (0.2%) of all blood cells. (Red blood cells vastly outnumber white blood cells.) B-cells, which are the cells on which vaccines act, are anywhere from one to twenty percent of all lymphocytes at any given time. This means that probably less than 0.004 % (or 4 in 100,000) of all cells in the blood are targeted by vaccines and can produce antibodies. In the generous (but highly unlikely) scenario that all T-cells might be stimulated and boosted by vaccines, that would raise the count to 0.1% (or one in one thousand) of all cells in the blood that would be stimulated by vaccines.

Vaccine manufacturers have focused, as they must in every vaccine for it to address advertised claims, on recognizable proteins produced by a pathogen. In the case of COVID, that protein is a spike protein. A second encounter with a pathogenic microbe, following either naturally acquired infection or the vaccine, arouses immunological memory. That subsequent encounter with a pathogen is a larger and faster response than in the first encounter. Often these are so fast and forceful that an individual can clear a virus before even being aware of its presence. This is an asymptomatic defeat of the virus. The stated goal of vaccination is for the vaccinated individual to experience no disease from the pathogen.
There are enormous and mounting problems with the use of vaccines against COVID. One of the earliest known problems is that vaccines against coronaviruses have never worked. [1] Other early problems with the COVID vaccines used in 2021 (from late 2020) include their hasty development and lack of animal trials and lack of informed consent and political and financial pressure to take vaccines. mRNA vaccines have had animal [2] and human trials, which failed abysmally. [3] The COVID vaccines were likely doomed to fail because they combined several known red flags for disaster: mRNA, lipid nano-particles (highly inflammatory), polyethylene glycol (PEG) (known to be highly and dangerously allergenic), and addressing a coronavirus. All of these four factors had been known to scientists in various fields to be very problematic already.
Then, compounding this growing catastrophe with the COVID vaccines, Professor of viral immunology Byram Bridle discusses how corners were cut, the phase three clinical trials were skipped, which forced the public on which the vaccines were used to become the phase three clinical trial subjects, of course, unbeknownst to them: “Those being vaccinated now are, whether they realize it or not, part of the phase three experiment.” [4] This is aside from the enormous problems now being learned regarding the lack of safety and lack of efficacy, in fact negative efficacy of these vaccines. [5]
For those of you who have not submitted to these vaccines, and even for those who have, I would suggest being very glad that vitamin D exists and is widely available. This article will examine effects of vitamin D, achieving far more protection of the human body in the adaptive immune realm than vaccines can even begin to achieve, and this has been amply demonstrated with regard to SARS-CoV-2 and COVID.
Adaptive immunity and Vitamin D
Vitamin D receptors have been found in abundance in activated lymphocytes. [6] [7] Whereas multiple lymphocytes contain vitamin D receptors, CD-8 lymphocytes, also known as cytotoxic T-cells, were found to have the highest concentration, and vitamin D was found to increase the number of those receptors. [8] However, vitamin D also regulates helper T cells, notably TH1, TH2 and TH17, as well as the regulatory T cells that play an essential role in the prevention of auto-immune disease, as discussed previously. Where vitamin D is deficient, T-lymphocytes are shown to be pathogenic. [9]
TH1 helper T cells tend to be more pro-inflammatory; their cytokines include interleukin (IL)-2, interferon gamma and tumor necrosis factor (TNF)-alpha, and vitamin D tends to suppress TH1, switching adaptive immune response to TH2. [10] For example, the vitamin D receptor (VDR) inhibits the T-cell cytokine IL-2. [11] In contrast, vitamin D tends to enhance TH2 helper T-cell proliferation and cytokine production. TH2 T-cells are more anti-inflammatory and those cells excrete such cytokines as the interleukins IL-3, IL4, IL-5 and IL-10. [12] [13]
Vitamin D3 has shown association with priming naïve human T cells, specifically CD4 and CD8 T lymphocytes, to enhance their migration to sites of infection. [14] The expression and activity of vitamin D receptors are important for every stage examined in the life of a T lymphocyte, including development, differentiation and expression of effector functions. [15]
Vitamin D vs viral infections
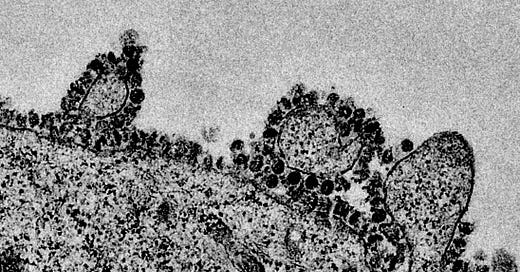
In the presence of pathogenic respiratory viruses, normal lung epithelial cells convert 25-hydroxy vitamin D (which is the inactive or storage form of vitamin D) to the active form, namely 1,25-hydroxyvitamin D3, which is the active form. [16] Cathelicidins are stimulated by vitamin D, and are essential to defense against viruses. Vitamin D also stimulates the powerful Type I Interferons (IFNs) which in turn stimulate expression of over 100 IFN stimulated genes, which show a variety of antiviral activities. [17] [18] Vitamin D also showed evidence of inhibiting viral replication. [19]
COVID has been compared to respiratory syncytial virus (RSV) in that both have shown life-threatening amounts of inflammatory chemokines in the airways. In both diseases, this process has been a part of its pathogenesis, severity of the infection and mortality. [20] Modest improvement in each is obtainable with prescribed corticosteroids, [21] but vitamin D gave more consistent response in RSV treatment. [22] Even the intractable human immunodeficiency virus (HIV-1) has shown susceptibility to Vitamin D treatment. [23] [24]
Significantly improved outcomes of respiratory infections have been seen with vitamin D supplementation and / or higher serum levels, in terms of shorter hospitalization, lower cost of care and lower mortality. [25] [26] In a study of 18,883 individuals, there was an increased prevalence of upper respiratory tract infection in those having less than 30 ng/ml serum levels of 25-hydroxy vitamin D compared to those having 30 ng/ml and above. This association was even stronger than season, body mass index, history of asthma or smoking or chronic obstructive pulmonary disease (COPD). [27] Pneumonia patients with < 12 ng/ml 25-hydroxy vitamin D levels had higher mortality at 30 days. [28] Children also showed correlation between low vitamin D levels and pneumonia and acute lower respiratory infection. [29] [30] Likewise, vitamin D deficiency in children was associated with more likelihood of hospitalization, severity of disease and longer hospitalization for respiratory infections. [31]
In the next part in this series, I will show the successfully life-saving results that vitamin D has shown against SARS-CoV-2, COVID and its variants.
[1] C Tseng, E Sbrana, et al. Immunization with SARS Coronavirus vaccines leads to pulmonary immunopathology on challenge with the SARS virus. Apr 20 2012. PLoS One. 7 (4). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3335060/
[2] M Zhang, J Sun, et al. Modified mRNA-LNP vaccines confer protection against experimental DENV-2 infection in mice. Sep 11 2020. Mol Therapy Methods & Clin Dev. 18: 702-712. https://www.sciencedirect.com/science/article/pii/S2329050120301625
[3] F Arkin. Dengue vaccine fiasco leads to criminal charges for researcher in the Philippines. Apr 24 2019. Science. https://www.science.org/content/article/dengue-vaccine-fiasco-leads-criminal-charges-researcher-philippines
[4] B Bridle. Coronavirus vaccine concerns: “I would prefer to have natural immunity.” Feb 24 2021. Dryburgh.com. https://dryburgh.com/byram-bridle-coronavirus-vaccine-concerns/
[5] C Huber. Trading COVID for heart disease buys you both. Jan 11 2022. Substack.
[6] S Manolagas, D Provvedini, et al. Interactions of 1,25-dihydroxyvitamin D3 and the immune system. Mol Cell Endocrinol. Dec 1985. 43 (2-3). 113-22. https://pubmed.ncbi.nlm.nih.gov/3000847/
[7] X Yu, H Mocharla, et al. Vitamin D receptor expression in human lymphocytes. Signal requirements and characterization by western blots and DNA sequencing. Apr 25 1991. J Biol Chem. 266 (12). 7588-95. https://pubmed.ncbi.nlm.nih.gov/1850412/
[8] R Wiese, A Uhland-Smith, et al. Up-regulation of the vitamin D receptor in response to 1,25-dihydroxyvitamin D3 results from ligand-induced stabilization. J Biol Chem. 267. 20082-20086. https://pubmed.ncbi.nlm.nih.gov/1328192/
[9] M Cantorna. Mechanisms underlying the effect of vitamin D on the immune system. Cambridge Univ Press. Jun 2 2010. https://www.cambridge.org/core/journals/proceedings-of-the-nutrition-society/article/mechanisms-underlying-the-effect-of-vitamin-d-on-the-immune-system/91FB1F56494E909053590AE99E4C6DC4
[10] J Lemire, D Archer, et al. Immmunosuppressive actions of 1,25-dihydroxyvitamin D3: preferential inhibition of TH1 functions. J Nutr Jun 1995. 125 (6 Suppl). 1704S-1708S. https://academic.oup.com/jn/article-abstract/125/suppl_6/1704S/4730957?redirectedFrom=fulltext
[11] I Alroy, T Towers, et al. Transcriptional repression of the interleukin-2 gene by vitamin D3: Direct inhibition of NFAT//AP-1 complex formation by a nuclear hormone receptor. Oct 1 1995. Am Soc Microbio J https://mcb.asm.org/content/15/10/5789
[12] J Adams, M Hewison. Unexpected actions of vitamin D: new perspectives on the regulation of innate and adaptive immunity. Nat Clin Pract Endocrinol Metab. Jan 31 2008. 4 (2). 80-90. https://europepmc.org/article/PMC/2678245
[13] M Hewison. An update on vitamin D and human immunity. Clin Endocrinol (Oxf). Feb 29 2012. 76 (3). 315-325. https://europepmc.org/article/MED/21995874
[14] F Baeke, H Korf, et al. The vitamin D analog TX527, promotes a human CD4, CD25high, CD127 low regulatory T cell profile and induces a migratory signature specific for homing to sites of inflammation. Jan 1 2011. J Immunol. 186 (1). 132-142. https://www.jimmunol.org/content/186/1/132.long
[15] M Kongsbak, T Levring, et al. The vitamin D receptor and T cell function. Jun 18 2013. Front Immunol. https://www.frontiersin.org/articles/10.3389/fimmu.2013.00148/full#B8
[16] Hansdottir, M Monick, et al. Respiratory epithelial cells convert inactive vitamin D to its active form: potential effects on host defense. J Immunol. Oct 31 2008. 181 (10). 7090 – 7099. https://europepmc.org/article/PMC/2596683
[17] P Smith, G Lombardi, et al. Type I interferons and the innate immune response-more than just antiviral cytokines. Mol Immunol. Jan 12 2005. 42 (8). 869-877. https://europepmc.org/article/MED/15829276
[18] J Hiscott. Triggering the innate antiviral response through IRF-3 activation. J Biol Chem. Mar 28 2007. 282 (21). 15325-15329. https://europepmc.org/article/MED/17395583
[19] A Stoppelenburg, J von Hegedus, et al. Defective control of vitamin D receptor-mediated epithelial STAT1 signalling predisposes to severe respiratory syncytial virus bronchiolitis. J Path. 232 (1). 57-64. https://onlinelibrary.wiley.com/doi/abs/10.1002/path.4267
[20] A Hornsleth, L Loland, et al. Cytokines and chemokines in respiratory secretion and severity of disease in infants with respiratory syncytial virus (RSV) infection. Apr 30 2001. 21 (2). 163-170. https://europepmc.org/article/MED/11378497
[21] J Van Woensel and J Kimpen. Therapy for respiratory tract infections caused by respiratory syncytial virus. Eur J Ped. May 31 2000. 159 (6). 391-398. https://europepmc.org/article/MED/10867842
[22] S Hansdottir, M Monick, et al. Vitamin D decreases respiratory syncytial virus induction of NF-kappa-B-linked chemokines and cytokines in airway epithelium while maintaining the antiviral state. J Immunol. Dec 10 2009. 184 (2). 965-974. https://europepmc.org/article/PMC/3035054#R80
[23] E Villamor. A potential role for vitamin D on HIV infection? Nutr Rev. 64 (5). May 2006. 226-233. https://academic.oup.com/nutritionreviews/article/64/5/226/1910640
[24] R Connor, W Rigby. 1 alpha, 25-dihydroxyvitamin D3 inhibits productive infection of human monocytes by HIV-1 Biochem Biophys Res Comm. Mar 31 1991. 176 (2). 852-859. https://www.sciencedirect.com/science/article/abs/pii/S0006291X05802645?via%3Dihub
[25] A Braun, D Chang, et al. Association of low serum 25-hydroxyvitamin D levels and mortality in the critically ill. Crit Care Med. Mar 31 2011. 39 (4). 671-677. https://europepmc.org/article/PMC/3448785
[26] L Mathews, Y Ahmed, et al. Worsening severity of vitamin D deficiency is associated with increased length of stay, surgical intensive care unit cost, and mortality rate in surgical intensive care unit patients. Am J Surg. Feb 9 2012. 204 (1). 37-43. https://europepmc.org/article/PMC/3992708
[27] A Ginde, J Mansbach, et al. Association between serum 25-hydroxyvitamin D level and upper respiratory tract infection in the Third National health and Nutrition Examination Survey. Arch Intern Med. Jan 31 2009. 169 (4). 384-390. https://europepmc.org/article/PMC/3447082
[28] L Leow, T Simpson, et al. Vitamin D, innate immunity and outcomes in community acquired pneumonia. Respirology. Apr 30 2011. 16 (4). 611-616. https://onlinelibrary.wiley.com/doi/full/10.1111/j.1440-1843.2011.01924.x
[29] L Muhe, S Lulseged, et al. Case-control study of the role of nutritional rickets in the risk of developing pneumonia in Ethiopian children. Lancet. May 31 1997. 349 (9068). 1801-1804. https://europepmc.org/article/MED/9269215
[30] V Wayse, A Yousafzai, et al. Association of subclinical vitamin D deficiency with severe acute lower respiratory infection in Indian children under 5 years. Eur J Clin Nutr. Mar 31 2004. 58 (4). 563-567. https://www.nature.com/articles/1601845
[31] J McNally, K Menon, et al. The association of vitamin D status with pediatric critical illness. Pediatrics. Aug 5 2012. 130 (3). 429-436. https://europepmc.org/article/MED/22869837




Your ignoring the important part. There is no way the Fauci Gang can make a $1,000 a second on vitamin D.
Thank you….I love when people make sense.
What it is not effective against is showing up at the ER and letting them manage your COVID experience in 2020.