Street Meds for Cancer? Repairing the Liver After Fenbendazole
Cancer patients have come into our clinic after trying fenbendazole to shrink tumors, with disappointment that it had not worked and upheaval in their liver labs.
Fenbendazole, known on the street as “dog de-wormer for cancer” has been very effectively advertised for anti-cancer effect. Social media has let this urban legend loose to the point where it gained high hopes and very high profile attention. Even Joe Rogan, the world’s biggest broadcaster by far, recently touted it on a podcast for shrinking tumors.
But there are some misconceptions that Rogan missed, not having worked at a natural cancer clinic as I have for the last 17 years.
First, fenbendazole is an OTC veterinary medicine, and is therefore subject to much looser quality control than human pharmaceuticals. Because this is being sold by third party vendors on the internet, who are fenbendazole’s biggest cheerleaders, it is your guess as to what exactly is in the capsules you receive, and at what concentration, after exactly what kind of quality control.
What has been missing from the public conversation is that fenbendazole’s mechanism against cancer is as a weak chemotherapy drug. Like vinblastine and vincristine, it disrupts microtubule formation and microtubule activity. [1] The drug’s target is the molecule tubulin, which helps provide the skeletal foundation of microtubules, which are necessary in cell replication – for both normal cells and cancer cells. Cancers reproduce faster than normal tissue, so a long-standing chemotherapy strategy has been to create damage to cellular replication, which injures cancer cells earlier than it injures normal cells, but does injure all kinds of cells.
At first, fenbendazole’s effect on disrupting the cell cycle looked effective in the lab mice. [2] But then, sacrificing mice to examine tumors is not quite the same as taking responsibility for human cancer patients to get well, to survive their cancers and to stay in remission long-term.
The two big problems that we have seen at my clinic with previous fenbendazole use are the following:
1) For a cancer patient to rely on anything – especially just one monomolecular approach - that does not work effectively against cancer wastes valuable time. Doing that attacks cancer only strongly enough to make it mutate. Just like giving too little antibiotic to bacteria, giving a mild chemotherapy like fenbendazole to a cancer patient, buys time for the tumor to become resilient to this gentle nudge. The net result usually strengthens existing cancer. It is one of the worst strategies against cancer, from what I have seen over the years.
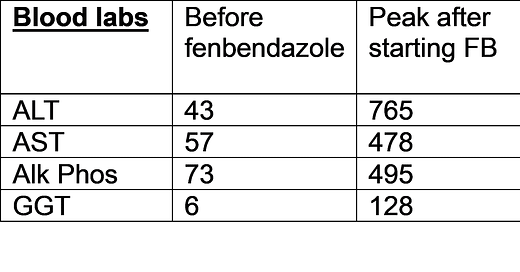
2) The other problem we have seen is that fenbendazole has not had good effect on the liver. There are reports in the medical literature of people damaging their livers with this drug, driving the liver enzymes ALT and AST into the several hundred range, but then reversing the alarming liver blood labs on discontinuation of the drug. [3] Alanine transaminase (ALT) and Aspartate aminotransferase (AST) are each supposed to be less than 40, and around the teens or 20 or so would be nice. This new liver toxicity may have potential to even begin new cancer in the liver. [4] The liver toxicity of another hepatotoxicant, acetaminophen, is increased when fenbendazole is added. [5] Besides liver damage, this study of fenbendazole use with pigeons showed multiple organ damage. [6]
At my clinic, people have arrived after trying a number of different conventional and / or natural, including dietary, approaches to cancer.
Here is a summary of liver blood labs in a patient who had chosen to take fenbendazole after recent public discussion of using it to attempt to fight cancer.
It should come as no surprise that fenbendazole and its metabolites mildly poison the liver. The related drugs mebendazole and albendazole are already known to have metabolites that are toxic to human livers, [7] by means of cholestatic liver injury, [8] and in dose-dependent effects. [9] This is why the usual course of mebendazole treatment in humans is only two days.
There are many effective substances against cancer, various routes to defeat it. Here are over 700 peer-reviewed studies on natural substances with effect against each of the major cancers.
Why not consider those treatments primarily that do not have a toxic profile, before considering ones that have little confirmed effect and are known to have a concerning toxic profile?
Joe Rogan did get ivermectin for COVID exactly right, [10] and has likely thereby saved countless lives, due to his enormous reach. But I must disagree with him regarding use of fenbendazole for cancer, on the basis of its unimpressive track record and primarily First Do No Harm.
March 20, 2024 update:
The pancreatic cancer patient who had the above lab values died within a few months after the liver damage that her doctors found at the time of fenbendazole use. Although the masses in the pancreas had decreased in size and perfusion with the clinic’s treatments prior to fenbendazole use, according to her medical records, the damage to the liver following fenbendazole use was thought by her doctors to be insurmountable and the cause of her death. We were told that that was on the urban legend dose that is popular online, without acetaminophen.
Please make sure that any cancer patient who considers such a toxin as fenbendazole has familiarized themselves with the studies below and the risks involved.
No clinic has ever posted better results than the documented results at our clinic, https://NatureWorksBest.com, and the reason for that is very simple: When a patient’s treatment choices remained among known effective cancer treatments within the non-toxic realm, a majority of patients went on to achieve remission. I explain why that is at length in the Cancer & Biochemistry videos under the tab at that same site. However, patients were of course always free to explore all of the toxic and invasive treatment options offered in conventional oncology at any time, before, during and / or after our clinic treatments.
[1] N Dogra, A Kumar, et al. Fenbendazole acts as a moderate microtubule estabilizing agent ad causes cancer cell death by modulating multiple cellular pathways. May 2018. Nature. https://www.nature.com/articles/s41598-018-30158-6
[2] W Wang, D Kong, et al. New Benzimidazole-2-urea derivates as tubulin inhibitors. Feb 2014. Bioorg Med Chem Letters. 24(17). https://www.sciencedirect.com/science/article/abs/pii/S0960894X14007598?via%3Dihub
[3] T Yamaguchi, J Shimizu, et al. Drug-induced liver injury in a patient with non-small cell lung cancer after the self-administration of fenbendazole based on social media information. Jun 2021. Case Rep Oncol. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8255718/
[4] T Shoda, H Onodera, et al. Liver tumor promoting effects of fenbendazole in rats. Sep 1999. Toxicol. Pathol. 27 (5). https://pubmed.ncbi.nlm.nih.gov/10528635/
[5] C Gardner, V Mishin, et al. Exacerbation of acetaminophen hepatotoxicity by the antihelminbthic drug fenbendazole. Feb 2012. Toxicol. Sci. 125(2). https://pubmed.ncbi.nlm.nih.gov/22048645/
[6] A Gonzalo, R Schwiebert, et al. Mortality associated with fenbendazole administration in pigeons (Columba livia) Nov 2006. J Am Assoc Lab Anim Sci. 45(6). https://pubmed.ncbi.nlm.nih.gov/17089995/
[7] G Choi, H Yang, et al. Acture drug-induced hepatitis caused by albendazole. Oct 2008. J Korean Med Sci. 23 (5). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2580005/
[8] Anthelmintic agents, in Liver Tox: Clinical and research information on drug-induced liver injury. 2012. National Inst Diabetes, Dig and Kidney Dis. https://www.ncbi.nlm.nih.gov/books/NBK548602/
[9] F Higa, K Kitsukawa, et al. Cytotoxicity of mebendazole against established cell lines from the human, rat and mouse liver. 1992. Arch. Toxicol. 66 (3). https://pubmed.ncbi.nlm.nih.gov/1497489/
[10] COVID-19 Treatment Research. Ivermectin for COVID-19: 230 ivermectin COVID-19 studies, 177 peer-reviewed, 99 comparing treatment and control groups. https://c19ivm.org/




Thanks Dr Huber. Wondering if you know the dosage/duration of the fenbendazole treatment that resulted in the liver enzymes your show in your table? First I've seen numbers for that though to be honest I haven't looked very hard.
"Why not consider those treatments primarily that do not have a toxic profile, before considering ones that have little confirmed effect and are known to have a concerning toxic profile?"
Can you list those, please?